Why I’m sharing this
My heart health journey wasn’t sparked by symptoms—but by concern. My brother, who shares much of my genetic makeup, fitness, and lifestyle history, experienced a serious cardiac event —despite having no symptoms.
Knowing our likely shared risk factors, and at my brother’s suggestion, I chose to get thoroughly tested—even though I felt strong, energetic, and symptom-free.
I’m glad I did get tested. What I discovered was both confronting and empowering.
A heart scan revealed a serious blockage - but my active lifestyle had already created a natural workaround.
Early Clues: Blood Tests, DNA and the Calcium Score
The first steps came through my partnership with the Australian Centre for Functional Medicine (AUSCFM) and its director, Rob MacPherson. I underwent extensive blood testing and a DNA analysis, which revealed multiple red flags (see the ‘What It All Meant’ section for simplified explanations):
- High cholesterol and fasting glucose (my cholesterol has always been at the high end of average).
- Type B LDL pattern and established atherosclerosis on my CT calcium score.
- Metabolic markers suggestive of cardiovascular strain.
- Genetic variations, particularly in the MTR/MTRR (methylation) and NOS3 (vascular function) pathways.
Together, these pointed to a higher heart risk—even in someone living an active lifestyle.
Then came the Coronary Artery Calcium (CAC) score.
My result—397—placed me in the 70th percentile, a moderate-to-high risk category. The CAC score only measures calcified plaque, which tends to be more stable, but its presence confirms long-standing atherosclerosis.
I still had no symptoms—but beneath the surface, the evidence was clear.
What It All Meant: Interpreting the Blood and DNA Clues
Lab results often seem technical, but here are the core findings that guided my heart health plan:
- Cholesterol Profile – low-density lipoprotein (LDL), often referred to as ‘bad cholesterol’:
Not all LDL cholesterol is created equal. My blood tests revealed a predominance of small, dense LDL particles (Type B), which are more likely to penetrate artery walls and contribute to plaque formation than the larger, more buoyant Type A particles. - Fasting Glucose – Borderline Elevated:
My blood sugar wasn’t in the diabetic range, but it was higher than ideal. Elevated glucose over time can damage blood vessels and increase the risk of atherosclerosis, especially when combined with other risk factors. - DNA Variations – MTR/MTRR (Vitamin Processing Genes):
These genes help your body use B vitamins like folate and B12 to keep blood vessels healthy and control a substance called homocysteine. If you have variations in these genes—like I do—your body may not process these vitamins as efficiently, which can quietly raise your risk for heart problems over time. - DNA Variation – NOS3 (Vascular Function):
This gene regulates the production of nitric oxide, which helps keep blood vessels open and flexible. My variant may reduce nitric oxide levels, potentially making blood vessels more prone to constriction and inflammation.
Understanding My Risk — What’s Genetic, What’s Lifestyle?
Although I’ve led a very active lifestyle, my test results made it clear that genetics played a major role in my cardiovascular profile.
It’s not always easy to separate what’s inherited from what’s lifestyle-driven—but here’s a summary of how each factor likely contributes, based on current science and my test results.
Likely Genetic Influences
- MTR/MTRR Gene Variants (Methylation Pathways):
These inherited traits affect how efficiently my body handles key B vitamins, subtly increasing risk over time by allowing homocysteine to rise. Homocysteine is a compound linked to vascular damage when elevated. - NOS3 Gene Variant (Vascular Tone Regulation):
A built-in reduction in nitric oxide production makes my blood vessels more prone to dysfunction—something I mitigate through regular training and nutrient support. - Small Dense LDL Pattern (Type B):
This cholesterol profile appears to be largely genetic in origin and is associated with increased plaque formation, regardless of lifestyle. - High Coronary Calcium Score:
This result, despite being highly active and having no symptoms, strongly suggests a genetic predisposition to plaque accumulation and inefficient cholesterol handling. - Family History – My Brother’s Cardiac Event:
A real-world signal that our family line carries a predisposition to coronary artery disease. His experience prompted me to dig deeper into my own risk.
Likely Mixed Genetic and Lifestyle Influences
- High Fasting Glucose (Metabolic Marker):
This may stem partly from genetic insulin sensitivity, but diet and muscle metabolism play a role. Thankfully, my strength training and balanced eating have helped me keep this in check. - Soft Plaque Presence (from Angiogram):
Soft plaques are more vulnerable to rupture and can’t be detected by a calcium score alone. Their formation is often tied to inflammation, oxidative stress, and metabolic dysfunction. Genetics play a role in susceptibility, but lifestyle choices—especially diet, exercise, and sleep—have a major impact on whether they worsen or stabilize.
Blood and DNA Analysis Conclusion
Put together, these clues showed that despite my active lifestyle and solid routine, my internal terrain wasn’t as protective as it looked from the outside. That insight became the springboard for the deeper cardiac testing that followed.
I may have inherited a cardiovascular risk profile, but my strength training, mobility, diet, and proactive health approach allowed my body to compensate in extraordinary ways, as detailed in the following sections.
Meeting the Cardiologist: More Tests
My GP referred me to a cardiologist for further investigation.
A CT Coronary Angiogram confirmed a 100% blockage in the Right Coronary Artery (RCA)—a major vessel whose obstruction can be life-threatening if not compensated for.
Another artery, the Left Circumflex (LCx), showed a 70–80% narrowing in its distal (far end) section—thankfully not near the origin, where blockages tend to be more critical.
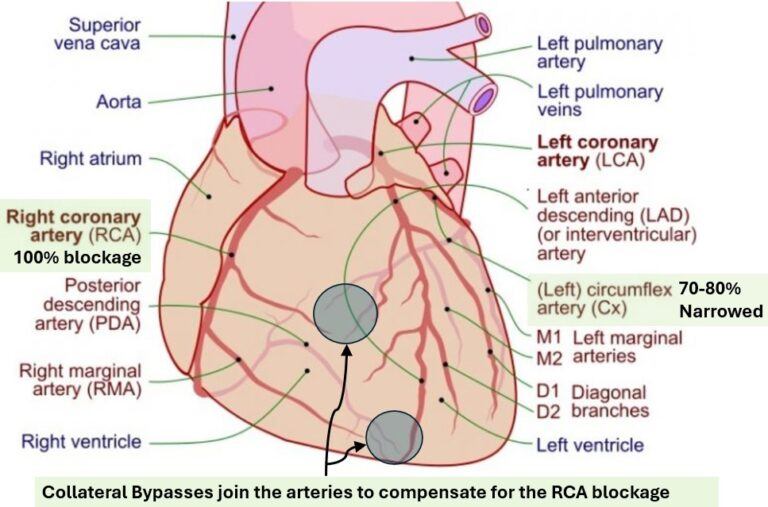
The diagram above shows my heart scenario (my comments in black text and in green shaded boxes):
- A 100% blockage in the Right Coronary Artery (RCA) artery,
- Significant narrowing in the Left Circumflex (LCx), and most importantly,
- The development of collateral arteries forming natural bypasses that maintained blood flow and likely spared me from a cardiac event.
At this stage stents or other invasive procedures were a real possibility..........but then came a surprising turning point: the stress echocardiogram.
During this treadmill test with before (rested) and after (exhausted) ultrasounds, I performed well above average for my age.
Based on published benchmarks I landed in the top 2 to 5 percent for my age group (born 1959). I reached my target heart rate around the 9-minute mark and kept going until 11 minutes, matching the average maximum for a healthy 35–40-year-old male.
Of course, many 35–40-year-olds (male and female) are fitter than I am—but based on the test metrics, my performance aligned with what’s typically seen in individuals 30 years younger.
Why Such a Positive Outcome?
This wasn’t luck.
My cardiologist acknowledged that my consistent resistance training, trekking, and active lifestyle likely played a critical role in the outcome—particularly in developing effective collateral arteries that rerouted blood flow around the blockage.
Rob MacPherson, Director of AUSCFM, adds:
“Weight training and muscle mass development play a pivotal role in overall health and longevity—especially in relation to heart health. Strength training supports metabolic function and helps prevent chronic diseases, including cardiovascular disease.”
I’m not taking any of this for granted and neither should you.
To gain insights into what's worked for me, see the other free website posts and go to the Membership drop down menu.
Become a member.
Watch this 2-minute video
Read the AD-Curve Free Post
AU$30 will unlock lifetime access to all current and future content, including 1 free 20-minute coaching call, extensive portable resistance training and mobility routines.
We also share tools and external resources that complement and align with our strength and mobility training approach — such as Movesmethod for mobility exercise and flow drills.”
My plan includes:
- Staying active with consistent strength training and regular walking / trekking during our travels
- Maintaining my medication and supplementation while monitoring their effectiveness
- Avoiding complacency with periodic testing and check-ins with my cardiologist
If you’re over 50—or not feeling quite right—don’t delay. Get tested.
I’m not chasing perfection—but I am committed to proactive aging with a long life and equally long health span.
Further Insights
What the Calcium Score Does – and Doesn’t – Show
While the CAC score is a reliable long-term risk marker, it only detects hard, calcified plaque—not the more dangerous soft plaque, which is prone to rupture, which can trigger sudden heart attacks.
In fact, people with a low calcium score have had heart attacks triggered by soft plaque rupture. My cardiologist acknowledged this and reinforced that cholesterol levels alone don’t tell the full story.
Some people with high cholesterol remain heart-healthy, while others with “perfect” numbers can still suffer events.
In my case, the angiogram revealed soft plaque as well—adding nuance to the risk picture and highlighting the importance of looking beyond the numbers.
Medications, Supplements and My Personal Routine
Medications – Every Day
My cardiologist prescribed two medications and recommended one supplement that I take in the morning every day.
- A statin, to help reduce the production of cholesterol and potentially stabilise existing plaque
- Low-dose aspirin, to reduce clot risk from ruptured plaque
- CoQ10, to support energy production in cells, especially important when taking statins, which can deplete CoQ10 levels
I had previously been cautious about medications. I’ve always preferred to think of these as ‘tools’ rather than ‘meds’—but appreciated my cardiologist’s pragmatic and supportive approach.
I didn’t need stents or surgery—but I was happy to support my body’s healing through smart interventions.
Alongside this, I continued with my supplement routine guided by AUSCFM and refined by personal experience as follows.
Additional Supplements – Every Day
- B-complex with methylation support – helps compensate for my MTR/MTRR gene variants and supports vascular health
- Magnesium powder – for muscle recovery, nerve function, sleep and cardiovascular support (magnesium also helps balance blood pressure)
- A Saw Palmeto supplement for prostate health
- Less rigorously, sometimes a multi-vitamin
Post Workout Supplements – Typically Every other Day
A mixture of Whey Protein Isolate and Creatine Monohydrate with a dissolved Immunity capsule.
The protein and creatine support muscle repair, lean mass, brain function and long-term functional strength. The Immunity capsule is an antioxidant and vitamin blend that supports immune resilience and energy, especially while travelling.
Together, these medications and supplements are part of an integrated, lifestyle-driven approach that supports energy, vascular health, and recovery—without working against the medical advice I’ve been given.
Feel free to email me and I will provide the supplement and medication brands that I use.
Final Thoughts: The Bigger Picture
You can’t always feel heart disease. I live an energetic, mobile, strength-focused life and I discovered a serious arterial blockage.
But thanks to the fitness foundation I’d built, my body had already adapted.
If you’re over 50—or have family history—don’t wait for symptoms. Talk to your GP and, if you are like me and want specific detailed analysis, contact AUSCFM about comprehensive blood work, DNA testing, and imaging.
And if you're training, walking, moving every day—know that you're doing more than building muscle or fitness. You could be building a backup system that one day saves your life.

Jeff, Very good information